Stretchable Electronics, Polymer Layers Key to Wearable Multifunction Medical Patch
Stretchable, flexible electronics are an attractive component for skin-attached sensors and monitors. A team at the Georgia Institute of Technology (Georgia Tech) has developed these electronics mounted on a substrate that can stretch with the medical film in which they’re embedded. Connected to gold, skin-like electrodes through printed connectors, the patch monitor can transmit electrocardiogram (ECG), heart rate, respiratory rate, and motion activity data up to 15 meters for the data analysis/reduction algorithms that extract these parameters from the sensed signals.
Because the device conforms to the skin, it avoids noise and artifact issues that normally occur due to the motion of the typical metal-gel electrodes across the skin. The device can even provide accurate signals from a person who is walking, running, or climbing stairs.
“When you put a conventional electrode on the chest, movement from sitting up or walking creates motion artifacts that are challenging to separate from the signals you want to measure,” said Woon-Hong Yeo, an assistant professor in the George W. Woodruff School of Mechanical Engineering and Wallace H. Coulter Department of Biomedical Engineering. He added that “because our device is soft and conformal, it moves with the skin and provides information that cannot be seen with the motion artifacts of conventional sensors.”
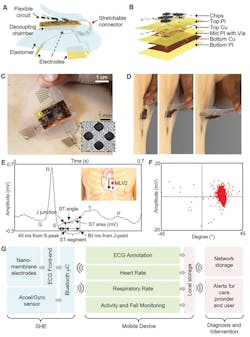
The major structural component of the stretchable hybrid electronic system (SHE) is a cast mixture of elastomers with extremely low moduli, so the device is naturally adhesive to the skin and compliant for stretching and bending (Fig. 1). This eliminates the need for conductive gels and adhesives, which add complicating issues of applying the patch and user comfort.
1. Overview of the SHE and data management showing: main structural components and their assembly for SHE (a); blow‐up image detailing the layer information of the flexible circuit (b); photo of an SHE showing the soft and adhesive property for direct lamination with the skin without the use of adhesives (c); side view of delamination sequence of the ultra-thin device with no negative effects to the skin (d); detailed inspection of ECG acquired by the SHE in (c) and identification of PQRST waves, J‐point, and ST‐segment angle (inset diagram describes the position of SHE (red dot) and polarity of the two measurement electrodes) (e); scatter plot (f) showing the angle and amplitude distribution of ST‐segments of the ECG data in (e); flow‐chart illustration of a real‐time, smart, and ambulatory health monitoring, enabled by the SHE (g). (Source: Georgia Tech)
The extremely thin Au/PI electrodes (1.2 µm) are arranged in a stretchable mesh layout that conforms to the complex skin surface structures, yet can easily deform along with the dynamic movements of the skin tissue. The integrated-circuit components are isolated by the elastomer and fully enclosed, and are powered by a lithium-based battery. The 500-µm-thick, low-modulus elastomer layer preserves the thin‐film properties of the nanomembrane Au electrodes and allows for the stable monitoring of the skin potentials.
Assembly of the wireless “all-in-one” SHE has four major steps:
1. Fabrication of the thin-film circuit and nanomembrane electrodes.
2. Transfer of the thin-film structures to elastomeric substrates.
3. Circuit assembly by reflow soldering of the surface-mount components.
4. Final packaging including electrode connection, elastomer encapsulation, creation of an oil chamber, and magnet attachment for the battery connection.
The set of three nanomembrane gold electrodes that contact the skin are photolithographically patterned into a network of repeating units of circular islands bridged with meander lines, for both stretchability and conformal contact to the skin.
The oil chamber seems like an odd part of the structure, but the need for it arose as a result of real-word issues and was deemed a practical solution. The researchers found that portions of the SHE soldered with the surface-mount chips would disrupt the compliant-device mechanics, leading to poor device and electrode adhesion. To overcome this, they added a thin oil-filled decoupling chamber under the circuit’s footprint to separate the mechanics between the electrodes and electronics. Vegetable oil was injected in the chamber using a micropipette and sealed with elastomer.
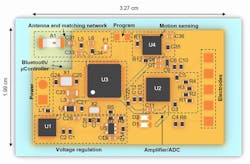
The circuit board, approximately 2 × 3.25 cm, includes electrodes, amplifier/ADC, motion sensing, voltage regulation, Bluetooth/microcontroller, and antenna and matching network (Fig. 2).
2. Top-view illustration of SHE’s circuit component with key functional blocks. A detailed BOM of the surface-mount components is in Table S1 of the Supporting Information. (Source: Georgia Tech)
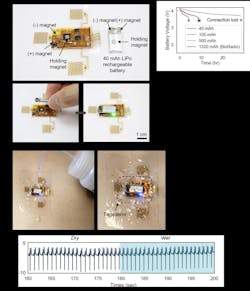
Magnets were used to hold and connect the 40 mA-hr Li-polymer rechargeable battery (Fig. 3).
3. The magnetic integration of the battery and waterproofing strategy includes details of the placement for the neodymium magnets for holding and connecting the battery (a); battery life tests with various capacities—average efficiency of the SHE is 0.1 hr/mAh (the data for the 500-mAh battery is cut off at 30 hours due to the limitation in the recording system) (b); a layer of Tegaderm can be applied over the circuit for continuous acquisition of physiological data during showering (c); the ECG measured before and after the application of water (d). (Source: Georgia Tech)
The device was tested both for durability and performance. For the former, numerous tests were run using various test-fixture arrangements, such as applying the patch to a soft cylinder (simulating an arm) and rolling it across a flat surface to physically stress the elastomers and circuitry. Field tests were conducted using test subjects. The raw physiological data was transmitted via Bluetooth to the connected mobile Android device, where it was processed through convolutional neural network (CNN)-based deep-learning algorithms to determine ECG, heart rate, respiration rate, and overall activity (Fig. 4).
4. In vivo, real‐time validation of the designed algorithms with human subjects including a real‐time, ambulatory monitoring of ECG and motion activity with a SHE on a human subject. At both idle (a) and active movements (b) of a subject, the device clearly detects VEB in the annotation model, with a variety of activities including walking, climbing stairs, and running (b). The four zoom‐in plots in (b) show a detailed two-second window of ECG waveforms from corresponding activity. (Source: Georgia Tech)
The design, fabrication, algorithms, and evaluations are described in detail in their paper “All-in-One, Wireless, Stretchable Hybrid Electronics for Smart, Connected, and Ambulatory Physiological Monitoring,”published the journal Advanced Science. There are also links to several videos at the end of the web-based, non-PDF version (both web version and PDF are posted). Extensive additional details—especially related to the electronics—are in their posted Supporting Information PDF document.
This research was supported by a grant from the Imlay Innovation Fund at Children’s Healthcare of Atlanta, NextFlex (Flexible Hybrid Electronics Manufacturing Institute), and the Georgia Tech Institute for Electronics and Nanotechnology, a member of the National Nanotechnology Coordinated Infrastructure, which is supported by the National Science Foundation.