Research Insights: Biomedical engineers shine light on blood-glucose levels
“Noninvasive glucose sensing is a Holy Grail of diabetes mellitus management,” write Professor Vladislav Yakovlev and his coauthors at Texas A&M University’s Department of Biomedical Engineering.1 “Unfortunately, despite a number of innovative concepts and a long history of continuous instrumental improvements, the problem remains largely unsolved.” That, however, may be changing, based on the Texas A&M researchers’ work developing an optical-detection technology that could monitor blood-glucose levels.
Their efforts build on research into diabetes that extends back at least to 1552 B.C., when the Egyptian physician Hesy-Ra identified symptoms of frequent urination and emaciation. Over the centuries, “water tasters” diagnosed the disease based on whether a patient’s urine tasted sweet. In the 1800s, chemical tests were developed to measure sugar in urine.2
Courtesy of Texas A&M University
Blood glucose test strip
However, urine testing had a number of drawbacks—for example, fluid intake affected test results—and blood testing became the preferred method of measuring glucose concentrations after the development of a blood glucose test strip (called Dextrostix) in the 1960s at the Miles-Ames Laboratory. The strips had their own drawbacks—such as color fading and variations in color assessment—leading to the search for an automated test-strip reader.3
Research in the 1960s led to the introduction of the Ames Reflectance Meter (ARM) in 1970, a portable 1.6-kg device with rechargeable batteries that could be used in doctors’ offices and hospital emergency departments. Subsequent improvements have led to the many portable meters available today for home use—including ones with wireless connectivity.4
S. F. Clarke and J. R. Foster of the History Committee at the Institute of Biomedical Science in London provide a list of developments in the evolution of self-monitoring blood-glucose systems, including the 1980 Ames Dextrometer, which included a digital display; the 1986 Ames Glucometer M, which could store results; the 1997 Bayer Glucometer Esprit, which could download results to a personal computer; and the 2002 Roche AccuChek Voicemate, which could assist visually impaired patients.3
But despite efforts at developing noninvasive glucose testing methods, the predominant test method today continues to require a finger prick to obtain the drop of blood needed for the test strip. Consequently, says Yakovlev at Texas A&M, patients can fail to self-administer the tests in accordance with typical three-time-per-day instructions. What’s more, the tests don’t provide real-time continuous monitoring.
Light absorption by glucose molecules
That’s what the Texas A&M researchers hope to change. They have demonstrated what they call “… the first successful implementation of a novel strategy based on vibrational overtone circular dichroism absorption measurements.” Their approach employs short-wavelength infrared excitation (1,000 to 2,000 nm) and determines glucose concentrations by measuring how glucose absorbs right and left circular-polarized light at the molecular level.
According to Yakovlev, the small but measureable effect is due to a geometric property of the glucose molecule known as chirality, which results in a glucose molecule absorbing light in a specific way. The specificity enables glucose molecules to be discriminated from other surrounding biological molecules, overcoming what Yakovlev calls the calibration problem. In addition, the approach reaches the penetration depths necessary to keep water in tissue from masking the glucose molecules.
“This technology has the potential to separate the presence of glucose from its surroundings, avoiding the calibration problem while circumventing the huge absorption of water in the fundamental vibrational region of the spectrum, allowing for clinically relevant penetration depths in biological tissue,” says Yakovlev in a press release posted at Newswise.
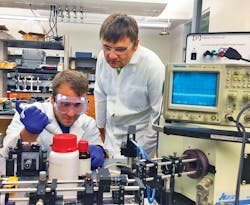
The researchers presented their findings—spearheaded by undergraduate student Carlos Tovar, under the guidance of Yakovlev and graduate students Brett Hokr and Zhaokai Meng—at this year’s SPIE Photonics West conference, where they reported using Monte Carlo simulations to show the feasibility of their approach. They currently are refining the technology in the laboratory and hope to move on to human trials. They note that one day the technology might be implemented in wearable devices such as smartwatches and bracelets.
References
- Yakovlev, V. V., et al., “Novel approach for non-invasive glucose sensing using vibrational contrast CD absorption measurements” (Invited Paper), SPIE Photonics West, Technical Program, 2016.
- McCoy, K., “The History of Diabetes,” Everyday Health, Nov. 3, 2009.
- Clarke, S. F., and Foster, J. R., “A history of blood glucose meters and their role in self-monitoring of diabetes mellitus,” British Journal of Biomedical Science, 2012.
- Lecklider, T., “Monitoring Blood Glucose Levels,” EE-Evaluation Engineering Online, July 20, 2015.