Electronics have been used to monitor and image patients for decades, with many advances arriving in the last 10 to 15 years. Technologies such as dual-mode medical scanners, wearable cardiac monitors, and even cameras that you swallow are helping physicians to quickly diagnose and treat illnesses.
With the inability for most doctors to visit patients and many more seniors wishing to stay in their homes, new technology will help keep individuals in their homes longer. Telemedicine relies on low-cost, portable medical monitoring systems located right in our homes.
A New Kind Of House Call
If you ask people if their doctor makes house calls, they will most likely say no—with a cynical look on their face. With the rising cost of healthcare, the average physician can no longer afford to travel to check on patients. Most people must travel to an office or clinic to see a physician or nurse practicioner.
Related Articles
- Get Your Prescription For Personal Medical Electronics
- Interview: Teresa Sanders Discusses TI Tech That Helps Parkinson's Patients
- Build A Wrist Heart-Rate Monitor Using An Ultra-Low-Cost MCU
But with the Internet of Things where even the smallest devices are connected to the Internet, there is a movement to once again bring the doctor to the patient (see "Wireless Networks Drive The Connected World"). The difference is that these visits will occur remotely via portable low-cost medical monitoring equipment located in the home. To accomplish this, though, several things need to take place.
First, monitoring equipment must be portable and accurate, and it must have a persistent connection to the Internet. The connection can be wired or wireless, depending on the device. But in most cases, it will require low power consumption, which is critical to battery-powered systems.
Second, the cost of the equipment (or possibly care provider services) must be reasonable for the masses. Equipment for blood glucose monitoring, ECG, pulse oximetry, and more can be monitored remotely, but it must be simple to use and fairly agnostic to user error.
The connectivity component is fairly straightforward. These interfaces are already available as chips or modules, allowing designers to easily equip devices with standards such as 802.11 (Wi-Fi) that can directly connect to the Internet. This type of persistent connection is advantageous over an on-demand connection since wearable monitors can be periodically polled for trends. Additionally, erratic readings can be used to trigger alarms that may indicate the onset of a serious condition.
Data Accuracy
Engineers designing home medical equipment can leave much of the user interface complexity at the application end (controlled by the patient’s doctor or care provider). However, this equipment still must take accurate measurements to be of value. Errors in the quality of the data due to a poor design can render remote health management useless. A doctor must trust that the data (and trends the data provides) is accurate to the limits of the measurements. That is, it should be as good as measurements provided by professional grade equipment in the physician’s office.
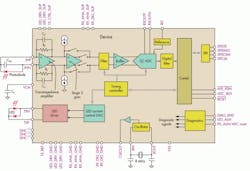
For example, a typical pulse oximeter works on the principle of photo-absorption of two wavelengths of light by arterial blood. This requires the system to drive two LEDs (red and infrared) in a fashion that allows the receive channel to discriminate between the signal and ambient light. The receiver uses a photodiode and requires a trans-impedance amplifier, gain stages, filters, and a very wide dynamic range precision analog-to-digital converter (ADC). The combination of all of these components uses a great deal of space and is costly.
Building small, connected devices that are simple for the patient to operate and cost-effective requires a high level of integration. Designed for heart-rate monitors and pulse oximetry measurements, the AFE4490 integrated analog front-end (AFE) integrates the entire analog sensing front end into a single 6-mm2 device (see the figure).
In combination with a microcontroller and connectivity, the AFE4490 can provide the basis for a wearable pulse-oximetry system that continuously monitors patients and reports their blood oxygen levels and heart rate. The connectivity could be Bluetooth Low Energy (BLE) for a connection to a cell phone, which can relay the information to a remote server, or an 802.11 Wi-Fi connection or LTE module.
For more advanced heart monitors such as a portable (wearable) ECG device, wires must be connected directly to a patient to pick up the subtle electrical signals that drive the heart muscles. Due to the direct nature of the connection to a patient, the design must also include current-limiting resistors to prevent electrical shock due to circuit failure (or misuse). These series resistors add noise to the already weak signals requiring a very low-noise AFE.
Additionally, all channels must be simultaneously sampled to maintain phase coherency between the inputs. Amplifiers are also required to form the Wilson Central Terminal or Goldberger Central Terminals required by 12-lead ECG equipment. ECGs can provide respiratory readings through demodulation of the signals as well, and this too requires additional circuitry to implement.
Again, to keep cost and size under control, integration is the answer. Devices such as the ADS1298R integrate eight independent channels with the flexibility to create low-cost, connected 12-lead ECG devices. Like the connected pulse oximeter, this device would require a microprocessor and some form of connectivity allowing home patients (with some basic training) to connect themselves (or someone else) to a remote doctor. These devices also might be worn so data can be recorded for anomalies that occur only occasionally. If the devices are wireless using BLE, they could report directly to the doctor when the event occurred so the circumstances would be better understood.
The Future
Home healthcare and telemedicine will grow throughout the next 10 years. InMedical, a subsidiary of IMS research, predicts that 1.8 million patients worldwide will be serviced by telemedicine by 2018.1 This growth will increase as technologies for placing tiny laboratories on a chip become cost-effective, allowing even more remote testing such as urinalysis and other tests now requiring a trip to a facility. Additionally, in the U.S. the aging Baby Boomers are more likely to remain in their homes throughout their elder years and will rely on this technology to maintain a higher quality of life.
For example, sensors placed under a mattress can detect respiratory rates as well as sleep patterns. Physicians and family members can use this data to remotely monitor the health and wellbeing of their loved ones. Eventually, small wrist monitors could communicate many critical vital signs to physicians, enabling individuals to live unassisted.
Conclusion
The future of telemedicine is undeniable. The integration of key components will be required to facilitate low-cost, high-performance equipment. This includes the sensitive high-performance AFEs that touch the sensors and ultimately the patient, as well as the communications infrastructure to support the data. Many people will be able to continue their lives independently into their elder years while maintaining an improved quality of life. With the rising cost of healthcare, telemedicine, along with the underlying technology that enables it, will help keep the doctor in the house.
This file type includes high resolution graphics and schematics when applicable.
References
1. News release: Telehealth to Reach 1.8 Million Patients by 2017, InMedia, January 21, 2013.
2. For more information on telehealth solutions, visit www.ti.com/telehealth-ca.