Self-Powering Electric-Field Skin Patch Speeds Wound Healing
What you’ll learn:
- How an applied electric field for medical electrotherapy speeds wound healing.
- Creation of the self-powered, non-electronic electrotherapy patch.
- Results of the electrical and medical performance assessment of this patch, tested on mice.
Chronic wounds are open wounds that heal slowly, if they heal at all, and existing treatment options are relatively expensive and restrictive for the patient. Research has shown that electrotherapy—use of a modest, localized, external electric field—is an effective and complication-free technique for speeding healing wound closure. However, that technique can be awkward and costly, due to its reliance on bulky equipment that limits its clinical use. (There are other healing-accelerants in addition to electrotherapy, each with different practical and medical attributes.)
Under a DARPA grant, a multi-institute team lead by researchers at Columbia University and North Carolina State University, among others, has developed a water-powered, electronics-free dressing (WPED). It uses a flexible, biocompatible magnesium-silver/silver-chloride battery and a pair of stimulation electrodes. Upon the addition of water, the battery creates a radial electric field. (Note that this is not a skin- or sweat-powered energy-harvesting arrangement.)
Their approach is in sharp contact with other battery-free electrotherapy schemes which are powered by wireless RF transmission. Those systems require that patients be in the vicinity of a transmitting antenna (which obviously restricts patient mobility), require carefully designed transmission and receiving antennas, and rely on relatively bulky RF amplifiers, function generators, and advanced impedance-matching units.
Studies show that electrotherapy leads to increased cell migration, venous blood flow, and cell proliferation, all of which accelerate healing. However, achieving the best patient outcomes using this method requires daily treatment for several hours, typically for weeks at a time. Thus, the treatment arrangement tends to be very stressful for patients and often goes uncompleted.
How Does the Wound-Healing Patch Operate?
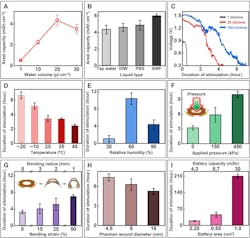
The wound-healing patch developed by this team includes a flexible, water-powered battery and a pair of thin-film stimulation electrodes seamlessly integrated with a commercial dressing. The battery produces an electrical field across the stimulation electrodes when activated with water (Fig. 1).
These water-powered dressings offer several hours of continuous stimulation with no restriction on patient mobility, robust performance (even under extreme temperatures, ambient humidity, and external pressures), and long shelf-life due to their materials, design architecture, and working principle.
Components of the Water-Powered Electronics-Free Dressing
The WPED involves a biocompatible magnesium-silver/silver-chloride (Mg-Ag/AgCl) battery (area: 0.64 cm2; weight: 47 mg; capacity: 0.4 mAh) affixed to the non-adhesive side of a commercial bandage (Tegaderm) and a pair of carbon-based stimulation electrodes on the adhesive side (facing the wound). The complete system (battery + electrodes + Tegaderm) is light (at 290 mg, only ~20% heavier than Tegaderm alone) and highly flexible for conformal attachment on curved body parts such as toes.
The battery, packaged within a polyethylene terephthalate film, is in an open-circuit, inactive state when the separator is dry. The separator includes an inlet pad where the user introduces water to activate the battery and a “check” pad to visually indicate complete hydration of the separator and successful activation of the battery.
When activated, the battery produces a voltage of about 1.5 V across the pair of stimulation electrodes, which include a central disk electrode connected to the anode (Mg; negative electrode) and an outer ring electrode attached to the cathode (Ag/AgCl; positive electrode). This configuration ensures a radial electrical field pointing to the wound center in line with the endogenous (meaning inside an organism or cell) electrical field, critical for promoting healing.
Testing the WPED
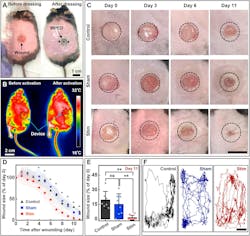
What about test and evaluation? Before testing “in vivo,” the biocompatibility of WPED was evaluated using NIH/3T3 mouse fibroblasts cultured with standard media, offering promising results in line with expectations. This was followed by in vivo tests using mice, where they evaluated the electrical and medical performance (Figs. 2 and 3).
Obviously, the metrics used for medical assessment are very different than those for electrical performance and involve statistical analysis and control groups. In brief, the WPED promoted healing by a meaningful and significant factor of about 30% by increasing epidermal thickness, modulating inflammation, and promoting angiogenesis (the process of new blood vessels forming from existing blood vessels in the body—good for wound healing, bad when related to cancer tumors).
The details of their work, including principles, materials, fabrication, dummy and in vivo tests, evaluation of data, and much more are in their lengthy yet highly readable paper “Water-powered, electronics-free dressings that electrically stimulate wounds for rapid wound closure” published in Science Advances.
About the Author

Bill Schweber
Contributing Editor
Bill Schweber is an electronics engineer who has written three textbooks on electronic communications systems, as well as hundreds of technical articles, opinion columns, and product features. In past roles, he worked as a technical website manager for multiple topic-specific sites for EE Times, as well as both the Executive Editor and Analog Editor at EDN.
At Analog Devices Inc., Bill was in marketing communications (public relations). As a result, he has been on both sides of the technical PR function, presenting company products, stories, and messages to the media and also as the recipient of these.
Prior to the MarCom role at Analog, Bill was associate editor of their respected technical journal and worked in their product marketing and applications engineering groups. Before those roles, he was at Instron Corp., doing hands-on analog- and power-circuit design and systems integration for materials-testing machine controls.
Bill has an MSEE (Univ. of Mass) and BSEE (Columbia Univ.), is a Registered Professional Engineer, and holds an Advanced Class amateur radio license. He has also planned, written, and presented online courses on a variety of engineering topics, including MOSFET basics, ADC selection, and driving LEDs.