Specialized pacemaker cells are found naturally in the heart. But if pacemaker cells go awry, the heartbeats slow down, causing fainting or even sudden death. Patients with slow heartbeats who are healthy enough to undergo surgery often look to an electronic pacemaker as their only treatment option. The implantable heart pacemaker, a triumph of engineering, has been helping keep alive millions of individuals since the first fully implantable pacemaker was given to a patient in 1958 at the Karolinska Institute in Solna, Sweden.
Since then, pacemakers have grown in sophistication and durability while also becoming a big business. According to a new report1 by Grand View Research, the global pacemaker market is expected to reach $12.3 billion by 2025. The growing prevalence of cardiac conditions and the availability of medical insurance coverage are key driving factors influencing the growth of pacemakers globally.
Meanwhile, though, innovators are not standing still. For instance, researchers at Rice University and the Texas Heart Institute (THI) recently showcased a wireless, battery-less pacemaker that can be implanted directly into a patient’s heart. The pacemaker, designed by the Rice lab of electrical and computer engineering professor Aydin Babakhani, receives power from radio frequency radiation transmitted from an external battery pack. In the prototype, the wireless power transmitter can be up to few centimeters away from the actual device.
This has important implications because pacemakers usually are not implanted directly into a patient’s heart. Instead, they’re placed where surgeons can periodically replace their onboard batteries with minor surgery. Short leads carry the actual impulses to the heart. However, all that wiring can lead to bleeding and infection, thus the “wire-less” approach of Rice’s prototype reduces these risks.
Although other lead-less pacemakers have been developed, their form factors limit them to a single heart chamber, and they are unable to provide dual-chamber or biventricular pacing. In contrast, battery-less, lead-less, and wirelessly powered microchips can be implanted directly to pace multiple points inside or outside the heart.
In a press statement, Dr. Mehdi Razavi, director of clinical arrhythmia research and innovation at THI and an assistant professor at Baylor College of Medicine, who collaborated with Babakhani on development and testing of the new pacemaker, noted, “This technology brings into sharp focus the remarkable possibility of achieving the ‘Triple Crown’ of treatment of both the most common and the most lethal cardiac arrhythmias: external powering, wireless pacing, and—far and away most importantly—cardiac defibrillation that is not only painless but is actually imperceptible to the patient.”
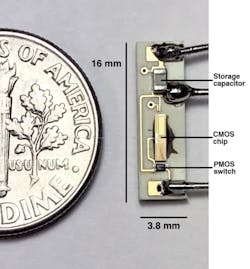
The chip at the system’s heart is less than 4 mm wide and incorporates the receiving antenna, an AC-to-DC rectifier, a power management unit, and a pacing activation signal. A capacitor and switch join the chip on a circuit board that is smaller than a dime. The chip receives power using microwaves in the 8-GHz to 10-GHz spectrum.
Wireless technology also is being employed in novel ways in Canada, where a medical team has implanted a wireless device inside a heart-failure patient, permitting clinicians to monitor the patient’s cardiovascular status—remotely and in real time—and proactively adjust treatment to prevent costly or potentially unnecessary hospitalization.
Funded by the Ted Rogers Centre for Heart Research, the device called CardioMEMS HF System was successfully implanted by interventional cardiologists at the Peter Munk Cardiac Centre in March 2017. The system features a small butterfly-like sensor that then sits inside the pulmonary artery of a heart-failure patient. When the patient lies on an accompanying antenna-equipped pillow device, the sensor provides important data—including the patient’s lung pressure readings—to clinicians, accessible to them via a secure website.
In parallel with the work of the engineer and the medical doctor, others are hard at work on making “devices” obsolete by harnessing nature.
Now, a $3 million grant from the National Institutes of Health to the Los Angeles-based Cedars-Sinai Heart Institute is helping investigators move closer to their goal of developing a biological pacemaker that can treat patients afflicted with slow heartbeats. Using minimally invasive gene therapy, a patients’ normal heart cells can be turned into pacemaker cells that regulate heart function—potentially replacing electronic pacemakers one day.
If the upcoming safety studies on the biological pacemaker are successful, Eugenio Cingolani, M.D., the principal investigator in the project, said the biological pacemaker could be tested in patients within the next five years.
Reference
- Global Pacemaker Market Size To Reach USD 12.3 Billion By 2025, Grand View Research, December 2016.
About the Author