How Will the Internet of Medical Things Change Healthcare?
This file type includes high-resolution graphics and schematics when applicable.
Technology has changed everything from the way television is watched, to the way we find directions, to the way we order food, but the medical industry has been surprisingly resistant to technology’s transformative effects—until now.
The convergence of cheap wireless transmitters, compact sensors, and low-power processors is driving the recent wave of fitness trackers, smartwatches, and wearable devices. While many of these wearables are aimed at the consumer market, a growing number of device makers are seeing the potential of wearable technology in transforming healthcare.
An increasing number of wearable medical devices, including skin patches, glucose monitors, and more, are shifting the focus of healthcare from the hospital to the home (Fig. 1). By allowing remote health monitoring, diagnosis, and even treatment, these wearable devices empowered by Bluetooth and NFC technology are changing the face of preventative medicine and the lives of those suffering from chronic disease.
Wearable Healthcare
Traditional healthcare has focused on the hospital and clinic as the center of patient care. Diagnosis and treatment all happen in the doctor’s office. Drugs and treatments are prescribed, but the doctor is unable to monitor or diagnose the patient until they come into the treatment center.
Telemedicine flips this dynamic, bringing healthcare to the patient’s home. Powered by the convergence of wearable devices, smartphone apps, and wireless connectivity, telemedicine is about bringing diagnostic and monitoring to the patient. Instead of having to wait for an appointment, today’s patients can use wearable medical devices to monitor and take charge of their own health.
Wearable devices have been life-changing for those with chronic disease like diabetes. Smart glucose monitors like the Dexcom G5 can be placed on the body and link wirelessly with smartphones to provide continuous blood-sugar monitoring. An app can alert users to low or high blood-sugar events, and can share data with loved ones or caregivers.
Quell is another example of wearable technology that’s changing the lives of those with chronic health issues. Using electrical nerve stimulation to relieve pain, it tracks activity and sleep patterns to adjust its pain-management intensity, as well as provide proactive relief throughout the night to improve sleep quality for patients dealing with chronic pain.
For elderly populations, wearables are improving quality of life by providing greater independence while ensuring safety. The UnaliWear Kanega is a prime example that combines a vital-sign monitor with an accelerometer and GPS tracking. It detects if elderly users have fallen and can transmit GPS coordinates as well as sensor information to loved ones.
Besides monitoring and notification, wearable medical devices also have the potential to provide automated or remote treatment. The OmniPod is an example of a wearable insulin pump that coordinates with a glucose monitor to automatically administer correct dosage. More drastically, ZOLL's LifeVest is a wearable defibrillator worn by patients at risk of a heart attack. It monitors heart rhythms and in the event of a heart attack, releases conductive gel from its electrodes and administers a life-saving electrical shock to restore normal heart rhythms.
More than just helping those already diagnosed with a disease, wearables are opening new possibilities in early detection and prevention of disease. Wearables with fitness and heart rate or EKG tracking capabilities are helping people maintain active lifestyles and track their heart health to ward off diabetes and heart disease.
While wearable medical devices vary greatly in shape, form, and function, they’re united by wireless connectivity that allows these compact devices to be worn unobtrusively. At the same time, wireless connectivity, especially Bluetooth Smart technology, allows these devices to connect with smartphones—sensor data can be analyzed through apps for self-diagnosis and shared with loved ones or caregivers.
Bluetooth Low Energy for Wireless Health
For wearable devices, Bluetooth Low Energy (BLE) is undoubtedly the most important wireless technology today. Not only is it power-efficient and easy to implement on embedded systems, but because of Bluetooth’s widespread compatibility, a BLE-supported device can be accessed by any modern smartphone made within the last three years.
Technically speaking, Bluetooth wireless technology consists of two separate sub-protocols. Bluetooth classic is the original Bluetooth wireless protocol designed for connecting headphones, speakers, and other devices that need to transfer significant amounts of data. Bluetooth Low Energy, also known as Bluetooth Smart, uses the same 2.4-GHz radio as Bluetooth Classic, but a significantly different stack implementation. Its messaging protocol is optimized for short, infrequent bursts of data instead of streams.
Bluetooth devices can either support Bluetooth classic, Bluetooth Low Energy, or both. Smartphones, laptops, and tablets generally support dual-mode Bluetooth, but for power-conscious wearables it makes sense to support just Bluetooth Low Energy.
Unlike other wireless protocols that may need a custom receiver module, with BLE devices, users can connect with their wearable simply through their smartphone with a compatible app. Subsequently, this data can also easily be shared with loved ones or caregivers through the phone’s 3G or 4G connection.
For hospital and home environments where Wi-Fi, Bluetooth, and other wireless devices on the 2.4-GHz band may be present, interference is a concern. Bluetooth Low Energy uses adaptive frequency hopping to select channels with less interference, allowing it to operate in noisy RF environments with Wi-Fi or other Bluetooth devices in the mix.
Power
Besides ubiquitous smartphone support, BLE also is an extremely power-efficient protocol. Peak power consumption when transmitting or receiving is much lower than Bluetooth classic. Transmissions and connection sequences are optimized for bursty messaging to significantly reduce messaging and connection times, and thus power requirements. While sending a sensor reading using a Bluetooth-classic device may take a hundred milliseconds as it connects and another hundred to send the data, the same process would take a Bluetooth Low Energy device just a few milliseconds.
Security
With wireless communications, security is always a concern. Bluetooth Low Energy employs 128-bit AES-CCM encryption, and since the release of Bluetooth 4.2 (released December 2014), it also uses Elliptic Curve Diffie–Hellman for key generation with strong protection against passive eavesdropping. For extra security against man-in-the-middle attacks, numeric comparison, passkey entry, or out-of-band pairing can be used.
Implementation
With the widespread popularity of Bluetooth, designers benefit from a range of cheap, integrated Bluetooth modules; well-documented, royalty-free BLE protocol stacks; and easy-to-use development kits. Many Bluetooth radio modules available today come in a SoC design with an integrated microcontroller that can also process sensor data and run application logic. For most medical wearables, this integrated approach will result in the smallest, cheapest, and most power-efficient end product.
Alternatively, for devices that need more processing power or memory (or is already available), Bluetooth Low Energy modules can also be interfaced through the standardized host controller interface (HCI) using UART or USB. In this case, the Bluetooth module is purely used for radio communications; the application and upper layers of the Bluetooth stack are run on a separate microcontroller. This allows devices with larger software footprints or processing requirements to use a separate, more powerful host processor and relegate the Bluetooth module purely for BLE communications.
One final benefit for BLE-driven wearable devices is over-the-air firmware updates. Many Bluetooth modules on the market today, such as those from Texas Instruments and Nordic Semiconductor, feature this capability. When device makers update their device with new capabilities, security patches, or bug fixes, users can easily download the firmware update through their smartphone and update their wearable wirelessly, with no USB cables required.
NFC: Tap-and-Go Technology
Bluetooth Low Energy, which maintains ubiquitous smartphone support, a usable real-world range of 10 to 30 meters that is perfect for indoor environments, and strong power efficiency, is the undisputed king of wireless communications for wearable medical devices. However, near-field communication (NFC) is a strong second-place contender. With an even smaller form factor, lower power usage, and tap-and-go functionality, it provides a complementary wireless technology with unbeatable ease of use.
Unlike Bluetooth, which lets users move around a room or area while staying connected, NFC requires devices to be within 10 cm, or practically touching, in order to activate. This physical limitation of NFC keeps it from being a direct competitor with Bluetooth, but is also the key to its value as a complementary wireless standard.
The close proximity of NFC connections allows for tap-and-go transactions that are quick and easy to initiate. Instead of choosing from a list of nearby devices and entering passcodes, users simply tap the devices together and it automatically triggers an NFC communication sequence. The intuitive nature of NFC is especially attractive for elderly populations, as well as for hospitals where it reduces or eliminates the need to train staff.
NFC’s maximum bit rate of 424 kb/s is much slower than Bluetooth Low Energy’s 1 Mb/s, but NFC interactions can still be quite fast. Two NFC devices can connect, transmit sensor data, and close the connection, all well within a second of the user touching the devices together. With Bluetooth, the same process could involve several seconds, as the user manually selects the correct device to pair with and initiates a sensor reading.
While it’s being built into ever-more smartphones, NFC’s main weakness is that it still doesn’t have the universal support like that of BLE. One way to get around this, an approach taken by Abbot’s Freestyle Libre glucose monitor, is to include a dedicated reader with the device. Device compatibility is also less of an issue in clinical settings, where compatible devices can be administered by staff.
In fact, in clinical settings, NFC may be better suited than BLE for many applications involving simple sensor readings and transactions, such as checking temperature or blood sugar, or transferring a medical record. Because of the ephemeral connections established by NFC, it works better than BLE when caregivers need to easily and quickly read multiple devices. Instead of establishing paired connections per device as with BLE, users simply tap their phone or tablet to each NFC device in turn to read it.
Besides acting as the main wireless transport, NFC also works well as a simple and secure handover to another longer range or higher bandwidth wireless protocol. NFC handovers are natively supported in the Bluetooth specification as an out-of-band pairing method, and can also be used to setup a Wi-Fi connection. This provides the simplified proximity pairing and authentication of NFC to Bluetooth or Wi-Fi connections. NFC connection handover is especially attractive in clinical settings where there may be dozens of active Bluetooth or Wi-Fi devices in connection range and connecting to the right one is critical.
Power
While Bluetooth Low Energy is extremely power-efficient, NFC can literally require no on-board power. NFC devices may be either active battery-powered devices, or passive devices. Passive NFC devices can be powered entirely by the RF field generated by an active NFC device connecting to it. This means extremely compact, completely battery-less designs are able to be made and used indefinitely. The power generated is typically around 4 mA at 3.3 V—enough for simple sensor readings.
NFC’s small size and ability to work purely off harvested RF energy makes it ideal for simple, compact wearables such as single-sensor skin patches, or electronic health record tags, both of which benefit from a small, flexible form factor and don’t need to perform complex sensor fusion or run application logic.
Security
By requiring devices to be in extremely close proximity, NFC provides physical security by making it extremely difficult to eavesdrop or create man-in-the-middle attacks. The close proximity also provides assurance that the correct device is being connected to, which simplifies pairing and authentication. For many applications, this provides a reasonable amount of security. However, for payment applications and applications transmitting sensitive information, Elliptical Curve Diffie-Hellman key exchange and AES encryption can be used for additional security.
Implementation
The NFC specification allows three modes of operation: peer-to-peer, read/write, or card emulation. Read/write, supported by simpler devices such as passively powered tags, allows for data to be written or read from a NFC device. This supports sensor readings applicable to medical wearables. Peer-to-Peer mode enables data exchange between two NFC devices, and is used for connection handovers and file transfers. With card emulation, an active NFC device can emulate a contactless smart card. This mode allows smartphones and active NFC devices to be used for payments or authentication applications, such as security access.
When it comes to NFC modules, designers have a huge range of options, from tags that store and transmit static data, to dynamic transponders that can be easily integrated with sensors, to multi-radio modules suitable for battery-powered devices.
Static NFC tags for healthcare can be used to store personal health records in a wearable wristband or keychain, making it easy for hospital staff or emergency personnel to check personal medical history, allergies, and drug contraindications.
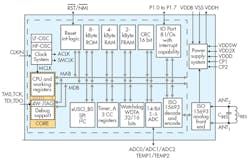
When passively powered, dynamic NFC transponders can be made extremely small, suiting them for skin patches or even implantable devices. NFC transponders like the TI RF430FRL152H (Fig. 2) are often specifically designed for these kinds of sensor applications, usually integrating an ADC and SPI/I2C interface, and with the ability to be passively powered.
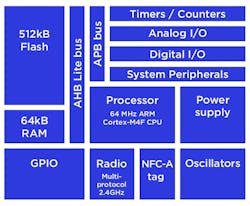
For battery-powered active NFC devices, multi-radio modules like the Nordic nRF51822 (Fig. 3) combine the ease of use and physical security of NFC with the range of other protocols. Bluetooth Low Energy + NFC modules are particularly compelling, as they combine the compatibility and range of BLE and the ease of use of NFC. Users with NFC-capable smartphones could exploit NFC to do a simple sensor reading or make a connection handover to Bluetooth for a more persistent connection. Users without generic NFC smartphones, such as those with iPhones, could still interact with the device, albeit in BLE-only mode.
The Internet of Medical Things
Simply put, wearable medical devices using Bluetooth Low Energy and NFC are transforming modern healthcare, improving the lives of the elderly, those living with chronic diseases, and those at risk of heart disease or other ailments. Monitoring solutions are reducing the occurrence of heart disease and diabetes, while automated treatment devices improve quality of life for those with chronic pain or illness.
Perhaps most promising of all, by connecting to our smartphones and tablets, the data provided by these wearables can enhance not only the health of the users themselves, but may help doctors and researchers better understand and treat the diseases and ailments that affect us all.